Navigating Hormonal Acne: Strategies for Managing Premenstrual Breakouts
Related Articles: Navigating Hormonal Acne: Strategies for Managing Premenstrual Breakouts
Introduction
With enthusiasm, let’s navigate through the intriguing topic related to Navigating Hormonal Acne: Strategies for Managing Premenstrual Breakouts. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Navigating Hormonal Acne: Strategies for Managing Premenstrual Breakouts

Acne, particularly the type that flares up before menstruation, is a common concern for many individuals. This premenstrual acne, often referred to as "hormonal acne," is driven by fluctuations in hormone levels, primarily androgen, during the menstrual cycle. While complete eradication may be challenging, implementing a multifaceted approach can significantly minimize breakouts and improve skin clarity.
Understanding the Hormonal Connection
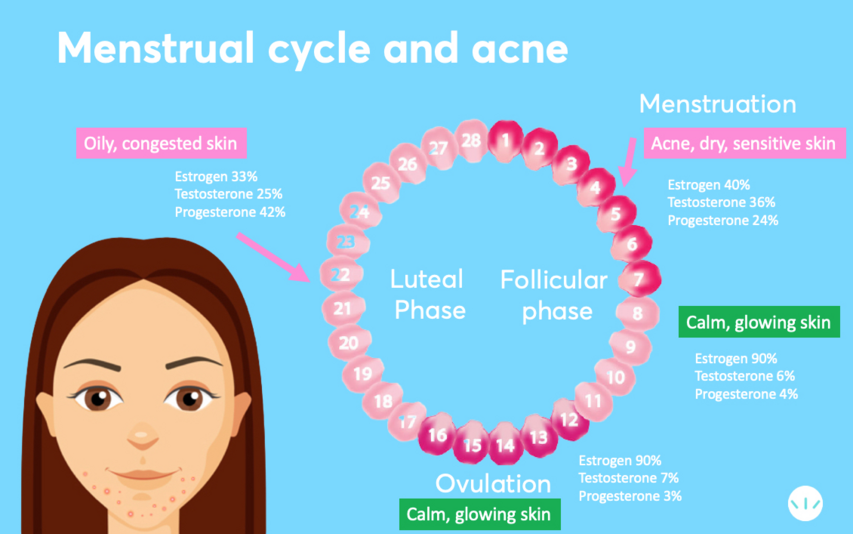
The menstrual cycle is a complex interplay of hormones, with estrogen and progesterone playing pivotal roles. As the cycle progresses, estrogen levels rise, leading to an increase in sebum production, the oily substance that lubricates the skin. However, as progesterone levels rise closer to menstruation, they can counteract the effects of estrogen, causing a sudden drop in estrogen and a subsequent surge in androgen levels.
This hormonal shift triggers a cascade of events that contribute to acne:
- Increased Sebum Production: Androgen stimulates the sebaceous glands to produce excess sebum, clogging pores and creating a breeding ground for bacteria.
- Inflammation: Increased sebum production leads to inflammation, causing redness, swelling, and pain associated with acne lesions.
- Keratinization: Hormonal fluctuations can also alter the shedding of dead skin cells, leading to a buildup of keratin within the hair follicles, further contributing to pore blockage.
A Multifaceted Approach to Premenstrual Acne Management
Addressing premenstrual acne requires a comprehensive approach that tackles multiple contributing factors. This involves:
1. Skincare Routine Optimization
- Gentle Cleansing: Opt for oil-free, non-comedogenic cleansers that remove excess oil and dirt without stripping the skin’s natural moisture barrier.
- Exfoliation: Regular exfoliation with gentle scrubs or chemical exfoliants helps remove dead skin cells and prevent pore blockage.
- Moisturization: While oily skin may seem counterintuitive, maintaining proper hydration is essential. Choose lightweight, oil-free moisturizers to prevent dryness and maintain the skin’s barrier function.
- Spot Treatment: Applying topical treatments containing benzoyl peroxide or salicylic acid can help reduce inflammation and kill bacteria within acne lesions.
- Retinoids: Topical retinoids, available by prescription, are highly effective in regulating sebum production and promoting cell turnover, reducing acne breakouts.
2. Diet and Lifestyle Modifications
- Dietary Considerations: Limiting processed foods, refined sugars, and dairy products can potentially reduce inflammation and improve skin health. Focusing on a balanced diet rich in fruits, vegetables, and whole grains can provide essential nutrients for healthy skin.
- Stress Management: Chronic stress can exacerbate hormonal fluctuations and contribute to acne. Engaging in stress-reducing activities like exercise, yoga, meditation, or spending time in nature can help manage stress levels.
- Adequate Sleep: Sleep deprivation can disrupt hormone balance and increase inflammation, potentially worsening acne. Aim for 7-8 hours of quality sleep each night.
3. Hormonal Management
- Oral Contraceptives: For some individuals, oral contraceptives can regulate hormone levels and reduce premenstrual acne. However, consultation with a healthcare professional is crucial to determine suitability and potential side effects.
- Prescription Medications: In severe cases, a healthcare provider may prescribe medications like spironolactone, which can block androgen receptors and reduce sebum production.
4. Professional Consultation
- Dermatologist Consultation: Consulting a dermatologist is crucial for personalized treatment plans and addressing underlying skin conditions that may contribute to acne.
- Gynecologist Consultation: A gynecologist can assess overall hormonal health and provide guidance on managing premenstrual acne through hormonal therapies or lifestyle modifications.
FAQs
Q: Can I use any type of cleanser for premenstrual acne?
A: It is essential to choose oil-free, non-comedogenic cleansers that do not clog pores. Ingredients to look for include salicylic acid or glycolic acid, which help exfoliate and reduce inflammation.
Q: What are some natural remedies for premenstrual acne?
A: While some natural remedies may offer mild benefits, it is crucial to consult a healthcare professional before using any herbal supplements or essential oils, as some can interact with medications or have potential side effects.
Q: How long does it take to see results from skincare changes?
A: It typically takes 4-6 weeks for changes in skincare routine to show noticeable results. Patience and consistency are key to achieving long-term improvements.
Q: Can I use makeup during premenstrual acne?
A: It is generally safe to use makeup during premenstrual acne, but it is essential to choose non-comedogenic products that do not clog pores. Avoid heavy, oily makeup, and opt for oil-free foundations and concealers.
Q: Can I prevent premenstrual acne completely?
A: While complete prevention may be challenging, adopting a comprehensive approach can significantly reduce the frequency and severity of premenstrual acne.
Tips for Managing Premenstrual Acne
- Keep a Skincare Journal: Tracking premenstrual acne patterns can help identify triggers and adjust your skincare routine accordingly.
- Don’t Over-Wash: Washing the face excessively can strip the skin’s natural oils, leading to dryness and irritation. Stick to a twice-daily cleansing routine.
- Avoid Touching Your Face: Touching the face can transfer bacteria and irritate the skin, potentially worsening acne.
- Protect Your Skin from the Sun: Sun exposure can worsen inflammation and hyperpigmentation, so always use sunscreen with an SPF of 30 or higher.
- Stay Hydrated: Drinking plenty of water helps flush out toxins and maintain skin hydration.
Conclusion
Premenstrual acne is a common concern that can be effectively managed with a multi-pronged approach. By understanding the hormonal factors involved, optimizing skincare routine, making lifestyle modifications, and seeking professional guidance, individuals can minimize breakouts and improve their skin clarity. Remember, patience and consistency are key to achieving long-term success in managing premenstrual acne.





![Hormonal Acne Treatment Guide [Updated 2021] Natural Acne Clinic](https://b940459.smushcdn.com/940459/wp-content/uploads/2020/08/Hormone-infographic-png-700x2283-copress-314x1024.jpg?size=696x2270u0026lossy=1u0026strip=1u0026webp=1)

Closure
Thus, we hope this article has provided valuable insights into Navigating Hormonal Acne: Strategies for Managing Premenstrual Breakouts. We appreciate your attention to our article. See you in our next article!